Once in a while new research is published on the effect of electromyography (EMG) as add on to pelvic floor muscle training (PFMT) in the treatment of urinary incontinence. However, the results of these studies are inconclusive meaning that both positive and no effects are reported.
I will discuss today’s study because it is well designed and compares ‘apples with apples’, meaning that the only difference in the intervention between the groups is the extra EMG. After reading this blog you will know why and how the research was designed and above all what the (main) results are and what this means in my opinion.
Why did they do this study?
This study aimed to assess whether pelvic floor muscle training with EMG (EMG group) is more effective than pelvic floor muscle training alone for the treatment of stress or mixed urinary incontinence.
How was this study done?
This is a multicentre (23 locations) randomized controlled trial. EMG group, n=295, pelvic floor muscle training group, n= 298.
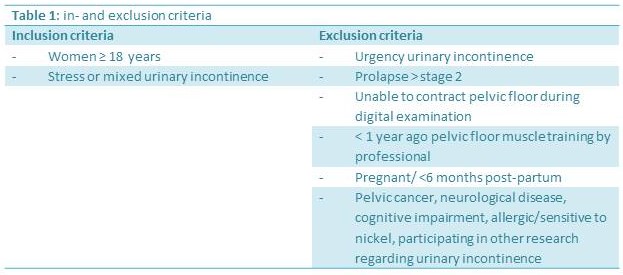
Participants: In- and exclusion criteria in Table 1.
Outcome measures:
- International Consultation on Incontinence Questionnaire-Urinary Incontinence Short Form (ICIQ-UI SF). Score 0-21 (0=no UI, 21=highest severity of urinary incontinence).
- Patient Global Impression of Improvement. One question, 7 response options (1=very much better – 7= very much worse).
- Subgroup analysis: 1. Stress or mixed urinary incontinence, 2. Age <50 or ≥50, 3. ICIQ-UI SF score <13 or ≥13 at baseline.
- Pelvic floor muscle function (strength, endurance (number of hold and repetitions)
Measurement moments:
- 6, 12 and 24 months
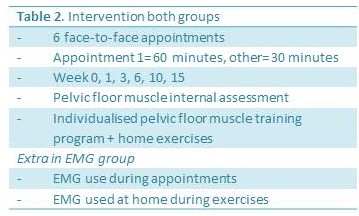
Intervention. Table 2
What are the results?
- There was no statistically significant difference between group at 6, 12 and 24 months regarding the ICIQ-UI SF.
- Subgroup analyses regarding type of urinary incontinence, age, baseline severity of urinary incontinence: no statistically significant difference between groups.
- Patient Global Impression of Improvement showed no statistically significant difference at 24 months.
- No differences between groups regarding: maximum muscle strength, contraction endurance and number of repetitions of the pelvic floor muscles.
By the way: these are just the main results. There is a lot more in the original article which is open access. Just use the link and discover the other resultsJ.
What does this mean for the pelvic physical therapist?
Pelvic floor muscle training with EMG is equally effective as pelvic floor muscle training alone. Therefore, in my opinion, the use of EMG in the treatment plan should not be standard and only be used in specific cases for a specific reason. A reasons to use EMG can be for instance the need to visualise the activity of the pelvic floor muscles, to motivate your patient to contract stronger, for a longer duration and to relax properly afterwards.
There is one thing that I missed reading this article. As described in Table 2 the pelvic floor muscle training was individualised. It consisted of a home trainings program aiming for 3 sets of exercises daily. I assume that both slow and fast contractions are part of the program. However, unfortunately the article does not describe functional training as part of the treatment plan. I think this is a pity because this is a very important part of pelvic floor muscle training in my opinion. And if functional training was a part, I am curious to know if the EMG group did their functional training while using the EMG to see how and when they contracted the pelvic floor muscles during for instance a jump.
Reference:
Hagen S, Elders A, Stratton S, Sergenson N, Bugge C, Dean S, Hay-Smith J, Kilonzo M, Dimitrova M, Abdel-Fattah M, Agur W, Booth J, Glazener C, Guerrero K, McDonald A, Norrie J, Williams LR, McClurg D. et al. Effectiveness of pelvic floor muscle training with and without electromyographic biofeedback for urinary incontinence in women: multicentre randomised controlled trial. BMJ. 2020 Oct 14;371:m3719. doi: 10.1136/bmj.m3719.BMJ. 2020. PMID: 33055247 Free PMC article.









Helemaal met je eens!