Up to 10%, an estimated 176 million, of women in their reproductive years are affected by endometriosis worldwide. Only a few women are diagnosed and treated. This means that pelvic physical therapist most likely see women with both diagnosed but also undiagnosed endometriosis. Pelvic pain (i.e. dyspareunia) is a common symptom of endometriosis.
Treatment can consist of hormonal treatment to reduce estrogen production and surgery to remove lesions. But why does pain return after surgery (or with hormonal therapy) in some cases without the existence of new lesions? The authors of the study I will discuss in this blog have previously published research that showed that pelvic sensitization and myofascial trigger points are more prominent in women with endometriosis and pelvic pain, compared to women with pelvic pain without endometriosis and healthy controls.
Why did they do this study?
The objective was to see if there is a pattern in distribution of myofascial trigger points and in cutaneous sensitization in women with pelvic pain and endometriosis.
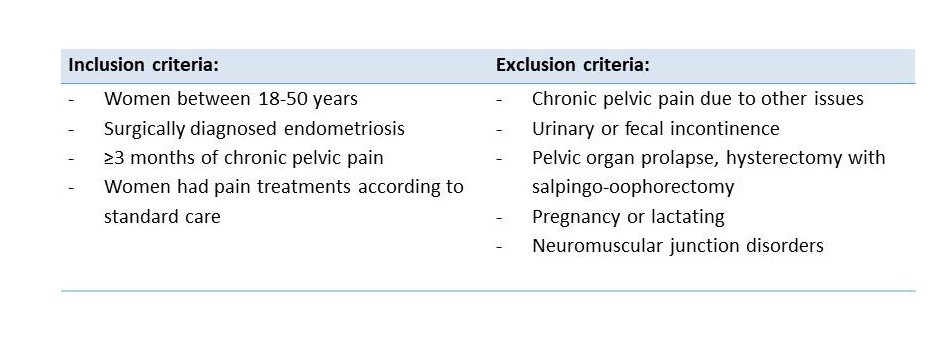
How did they do this study?
Examinations:
- Abdominopelvic palpation (tenderness and spasm)
- Muscles: pubococcygeus, iliococcygeus, obturator internus
- Bladder, urethra, uterosacral ligament, forniceal and vaginal wall pain
- Size uterus and adnexes, pain and mobility
- Neuromusculoskeletal
- Sacroiliac joints
- Abdominal myofascial trigger points (number, pain level)
- Derma- sclero- and myotomes (C2 to S2) for allodynia and hyperalgesia. Myotomes were checked with the 26 regions similar to assess fibromyalgia.
- Brief pain Inventory (BPI) for participant to indicate which body parts (total 71) were painful. Widespread pain = 10 or more pain territories.
CLASSIFIED AS:
MYOFASCIAL DYSFUNCTION = ≥7 myofascial trigger points on each side.
REGIONAL ALLODYNIA/HYPERALGESIA > half of dermatomes (C2-S2) on either side (≥12/23 segments) sensitization: local or widespread
What did this study find?
The results are based on 30 women (median age=30), with 2-25 years of pelvic pain (mean 11.5).
- Dyspareunia reported by 93% (14/15) of the women who had sexual intercourse the last month.
- 7/15 (46.7%) avoided intercourse because of pain.
- All participants had pelvic floor muscle spasm (ICS terminology: pelvic floor ‘hypertonicity’). In 77% of cases 4 out of 6 pelvic floor muscles provoked the reported pelvic pain.
- Pelvic pain: 67% (20/30) of participants reported focal pelvic pain and 33% (10/30) as diffuse, not localized.
- Abdominal pain: 57% in pelvic region, 40% no pain on palpation, 3% diffuse pain.
- Myofascial dysfunction: all women in >2/3 of 26 regions and of which 47% had myofascial trigger points in all 26 regions.
- In general low pressure pain thresholds of interspinous ligaments.
- 70% of the women reported orofacial pain or regular severe headaches (77%)
- Participants with > 10/71 painful body territories/BPI (n=10) reported more diffuse pelvic pain and had more widespread sensitization.
What do these results mean (for the pelvic physical therapist)?
This study showed that women with endometriosis have widespread myofascial dysfunction, lower pressure pain thresholds of interspinous ligaments and central sensitization. The central sensitization might explain the fact that some women after surgery of the lesions or hormonal therapy are still in pain. The authors hypothesise that ‘pelvic floor muscle spasm’ might act as a pain generator.
As a specialized pelvic physical therapist we have a lot of tools to treat chronic pelvic pain and/or be part of a multi-disciplinary team. Although this study has only 30 participants and larger studies are needed to confirm the results, it has very interesting results.
It shows the importance of a vaginal examination and an examination of myofascial trigger points of all regions (abdomen and spinal area’s) in patients with endometriosis and pelvic pain (dyspareunia). Although not a research question in this study, I wonder if we should investigate this also in women who we suspect might have (undiagnosed) endometriosis.
Reference:
V.T. Phan, P. Stratton, H.K. Tandon, N. Sinaii, J.V. Aredo, B.I. Karp, M.A. Merideth, J.P. Shah. Widespread myofascial dysfunction and sensitization in women with endometriosis‐associated chronic pelvic pain: A cross‐sectional study. European Journal of Pain. Accepted
16 December 2020. https://doi.org/10.1002/ejp.1713









Recent Comments