In this blog I will discuss a well-designed randomized controlled trial. The objective of the trial was to see whether combining behavioural therapy with drug therapy had a better result than behavioural or drug therapy alone in men with overactive bladder symptoms.
Overactive bladder syndrome (OAB) is defined by the International Continence Society(ICS) as urinary urgency, usually with urinary frequency and nocturia, with or without urgency urinary incontinence. The symptoms can be treated with drugs and/or behavioural interventions like physiotherapy. The behavioural therapy can consist of for instance pelvic floor muscle and bladder training. Drugs that are prescribed have different working mechanisms. The α-blockers work on the bladder outlet by reducing the smooth muscle tone and the group of antimuscarinics inhibit detrusor contractions.
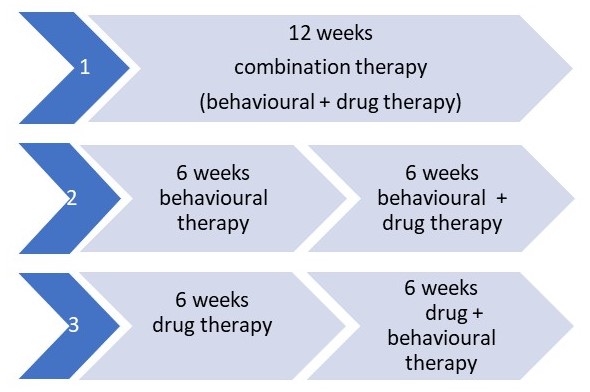
This study had the aim to compare 3 treatment options(figure 1):
Inclusion criteria:
- Men of ≥40 years
- 9 or more voids per 24 hours
Exclusion criteria:
were for instance: outlet obstruction, urinary tract infections, cancer (complete list in supplement of full text article)
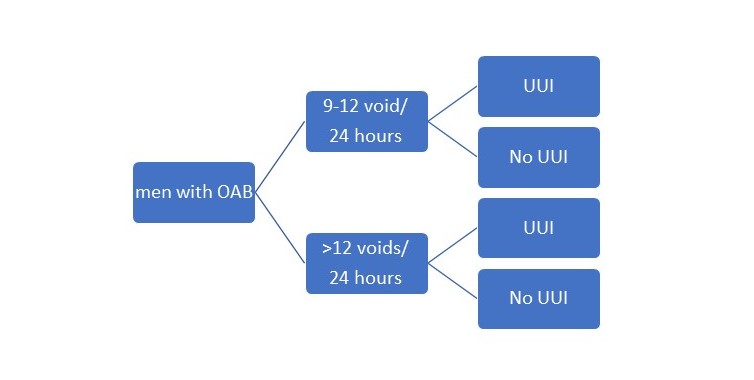
To ensure equal groups they made 4 different groups and randomized within these groups (figure 2)
Figure 2: randomization
TREATMENT
- Behavioural + drug therapy (combination): combination of the two therapies below.
- Drug therapy: Tolterodine (antimuscarinic) + tamsulosine (α-blocker). After 3 weeks the participants were asked about adverse effects and adherence to the medication.
- Behavioural therapy (3 sessions at baseline, 2 & 4 weeks): pelvic floor muscle training, bladder training/urge suppression techniques.
Pelvic floor muscle training: A correct contraction of the pelvic floor muscles was checked with anal palpation and observation of use of abdominal muscles. The duration of the contraction was based on individual ability to contract the pelvic floor muscles. It was increased up to a contraction of 10 seconds with equal resting time. The men had to perform 15 contractions, 3 times per day so 45 contractions in total.
Bladder training/urge suppression techniques: Postponing voiding, urge suppression techniques and advise to stop drinking 3 hours before they go to bed and during the night (nocturia).
MEASUREMENTS:
- Voiding diary (baseline, 6 weeks, 12 weeks) with Indevus Urgency Severity Scale for every void and incontinence episode.
- Overactive Bladder Questionnaire (symptom bother and health related quality of life)
- International Prostate Symptom Score (frequency of lower urinary tract symptoms)
- Patient satisfaction question:
- Patient perception of treatment outcome
- Estimated Percent Improvement
- Global Perception of Improvement
- Adherence to drug therapy and behavioural therapy.
Primary outcome:
- Voiding frequency
Secondary outcome:
- Urgency
- Incontinence
- Nocturia
RESULTS:
In total 204 men were randomized and included in the intention to treat analysis. In total 183 men completed the protocol.
- Behavioural therapy alone, n=71, 8 drop outs (mean age; 63.3)
- Drug therapy alone, n=68, 7 drop outs (mean age; 65.5)
- Combined therapy, n=65, 6 drop outs (mean age; 63.2)
At 6 weeks combined therapy showed the best result. However not significantly better than behavioural therapy alone. At 12 weeks the outcome for the 3 groups were the same (figure 3 and table 1).
Primary outcome: voiding frequency
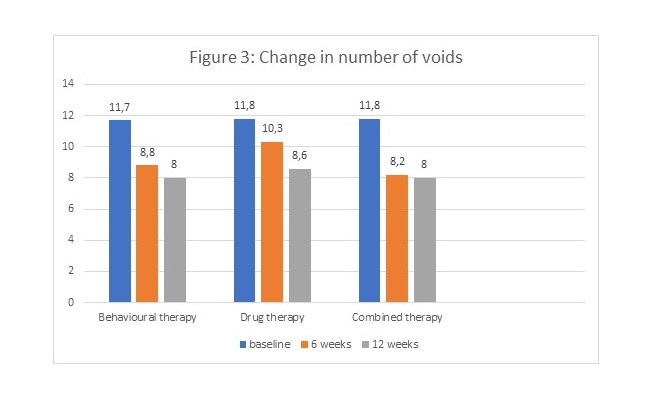
Table 1: percentage change:
|
|
6 weeks |
12 weeks |
|
Behavioural therapy |
24,7 |
31,6 |
|
Drug therapy |
12,7 |
27,1 |
|
Combined therapy |
30,5 |
32,2 |
Secondary outcomes at 12 weeks:
- Nocturia: Significant decrease in all groups. Best result in combined therapy, worst result in drug therapy alone.
- Mean urgency scores; significant decrease in combined therapy group. Not significant in behaviour and drug therapy alone groups.
- Incontinence; significant decrease in all groups. Combined therapy is superior. Baseline 6.6 episodes/week, 12 weeks 1.2 episodes/week (change 81.8%)
- Overactive Bladder Questionnaire and International Prostate Symptom Score; significant decrease in all groups. Combined therapy best result.
- Patient global ratings:
- Patient perception of improvement (better or much better): no difference between groups
- Percentage of patients completely satisfied after 12 weeks: no difference between groups
- Bothersomeness of adverse effects
no adverse effects + not at all bothersome;
- 6 weeks: behavioural therapy; 86%, drug therapy; 32%, combined therapy; 34%
- 12 weeks: behavioural therapy; 48%, drug therapy; 35%, combined therapy; 37%
Conclusion authors:
The combination of behavioural and drug therapy (combination group) had the best results at 6 weeks with regard to voiding frequency, nocturia and incontinence when compared with drug therapy alone. However there was no significant difference with the behavioural therapy alone. As the combination therapy had more adverse events than the behavioural therapy alone the authors state that starting with behavioural therapy in men with OAB is a reasonable choice. After the initial 6 weeks the men can discuss with their physician (shared-decision making) if they want to add drug therapy or not.
My personal opinion:
This is a well-designed randomized controlled trial confirming the positive effect of behavioural therapy for men with overactive bladder syndrome.
For us pelvic physiotherapists it is good to know that this research exists because we can discuss it with our referring physicians and answer questions of patients regarding drug therapy as well.
There is a lot more detailed information in the original article. So if you have access to the full-text article you can have a look at the exact numbers.
Reference:
Burgio KL, Kraus SR, Johnson TM 2nd, Markland AD, Vaughan CP, Li P, Redden DT, Goode PS. Effectiveness of Combined Behavioral and Drug Therapy for Overactive Bladder Symptoms in Men: A Randomized Clinical Trial. JAMA Intern Med. 2020 Jan 13. doi: 10.1001/jamainternmed.2019.6398. [Epub ahead of print]









Again I liked this abstract. I wanted to look at the full text but that isn’t possible, so I’ll ask this question here. In the RCT an inclusion criteria is 9 voids a day, but I am wundering how much they drank.
Thank you for your question. Fluid intake was not reported in the article.
Amazing Web site, Keep up the fantastic work. Thanks a lot!
Thanks for every other excellent post. Where else could anyone get that type
of information in such an ideal method of writing?
I have a presentation subsequent week, and I’m at the search
for such information.
Thanks for a marvelous posting! I genuinely enjoyed
reading it, you may be a great author.I will be sure to
bookmark your blog and definitely will come back later in life.
I want to encourage continue your great job, have a nice
day!
Hello there! Would you mind if I share your blog with my twitter group?
There’s a lot of folks that I think would really enjoy your content.
Please let me know. Cheers