Constipation is very common among stroke patients. Although it can affect for instance quality of life negatively it is often a forgotten subject. We know that the colon transit time is longer in poststroke patients with constipation. But we don’t know if rectal sensation and anorectal manometry are influenced.
The research I will discuss today has the following research questions:
- Is there a difference in anorectal motility and rectal sensation in stroke patients with constipation 2. Has the stroke site impact on constipation and rectal sensation
3. Are there independent risk factors for poststroke constipation
METHOD
For this study stroke patients and age- and sex matched healthy controls were included.
Inclusion criteria:
- Stroke
Exclusion criteria:
- Constipation before stroke
- Intestinal diseases in the past
- Abdominal operations other than appendectomy or cholestectomy
- Organic diseases like: spinal cord injury, traumatic brain injury, thyroidal dysfunction
- Pregnant or lactating women
Definition of constipation based on 2 criteria:
- Patients had to have at least 2 of the symptoms in at least 25% of defecations: straining, lumpy or hard stools, sensation of incomplete evacuation, sensation of anorectal obstruction or blockage, manual help to empty bowel, less than 3 spontaneous bowel movements per week.
- Loose stools hardly ever spontaneous.
Measurements
The stroke patients had to fill a 1 week bowel diary. There were questions on (spontaneous) bowel movements, Bristol Stool Form, time spent on toilet per defecation and the use of laxatives, digital help, number of successful defecations with straining, and successful defecations with the sensation of incomplete emptying.
Anorectal manometry: the patient was lying on the left side with knees and hips bent. The pressures of the rectum and anal sphincter were measured in rest, squeezing (3 attempts), and straining (5 attempts)
The anal inhibitory reflex and rectal sensation were measured.
Patient assessment of Constipation Symptom (PAC-SYM)
Modified Patient Assessment of Constipation Quality of Lify (PAC-QOL)
RESULTS
Seventy one patients were included, 34 (mean age 65.1) with and 37 (mean age 62.0) without constipation. On average 9 to 9.5 days after stroke. Roughly 75% were in the acute phase. No difference in number of men and women between the groups.
Patients with poststroke constipation had (significant):
- Less fluid intake (P=0.028)
- Less physical activity (P=0.026)
- > antihypertension medication and diuretics/dehydrants (P=0.006, P=0.01)
- > laxatives and suppositories
- < (spontaneous) bowel movements
- < Bristol Stool Form (P<0.001)
- > time in toilet
- > PAC-SYM 0.83 (0.58, 1.10) (P<0.001)
- > PAC-QOL 0.84(0.59,1.20) (P<0.001)
Anorectal sensation
Patients with poststroke constipation felt (all significant) the first sensation later, reported the desire to defecate and urge to defecate later compared to non-constipated patients and the healthy controls. There was no difference between the non-constipated and healthy controls (Figure 1).
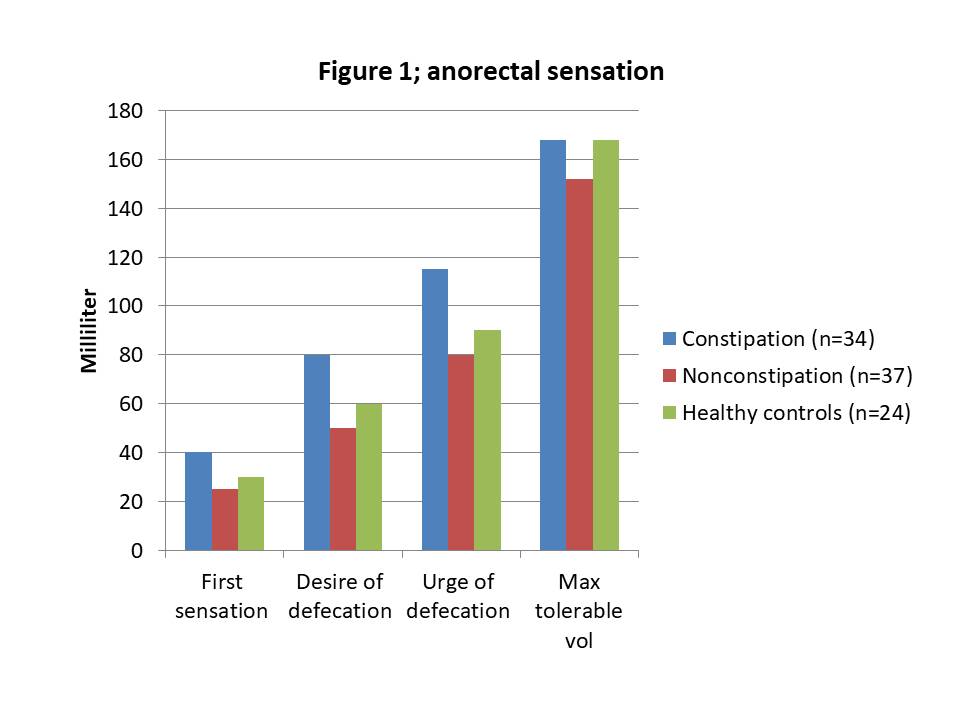
Impaired rectal sensation was weakly to moderately correlated with constipation.
Anorectal manometry
There was no significant difference between groups for anal resting pressure, maximal squeeze pressure and duration of contraction.
Increase in rectal pressure during straining was significantly less for the constipated stroke patients. There was no paradoxical contraction in any of the groups.
Location of stroke
Patients with brainstem lesions had significantly more constipation than those without. They also had higher threshold for first sensation compared to the non-brainstem lesions.
Independent risk factors
Independent risk factors for the development of poststroke constipation are:
- Higher threshold for desire of defecation (OR=1.079, P=0.047)
- Less physical activity (OR=0.992, P=0.025)
RELEVANCE OF THIS RESEARCH FOR PELVIC PHYSIOTHERAPIST
This is really interesting research showing that rectal sensation is compromised in poststroke patients with constipation. Patients with brainstem lesions are more at risk of developing constipation than other types of stroke. This means that there might be neural damage in patients with brainstem lesions. There was no sign of paradoxical contraction (dyssynergic defecation) in poststroke patients. It is well known that inactivity increases the risk of constipation. This research confirms this outcome.
As this is the first study researching poststroke rectal sensation more research is needed. In this study the majority of patients were in the acute phase so I hope that future research will prospectively follow patients to see if rectal sensation changes over time. More differentiation between types of stroke and constipation would be good as well.
I haven’t discussed the 4th research question, the exploration of autonomic function in this blog. If you want the outcome, please read the article.
There is (some) research suggesting that transcutaneous electrical acustimulation on a specific acupuncture point can improve rectal sensation. As far as I can see acustimulation is electrostimulation with surface electrodes placed on specific acupuncture points. This might be interesting for pelvic physiotherapists in the future. I am keeping a close watch on this and let you know as soon as there is more on this topic.
Reference:
Poststroke Constipation Is Associated With Impaired Rectal Sensation. Cheng J, Li L, Xu F, Xu Y, Lin L, Chen JDZ. Am J Gastroenterol. 2020 Jan;115(1):105-114. doi: 10.14309.








Recent Comments